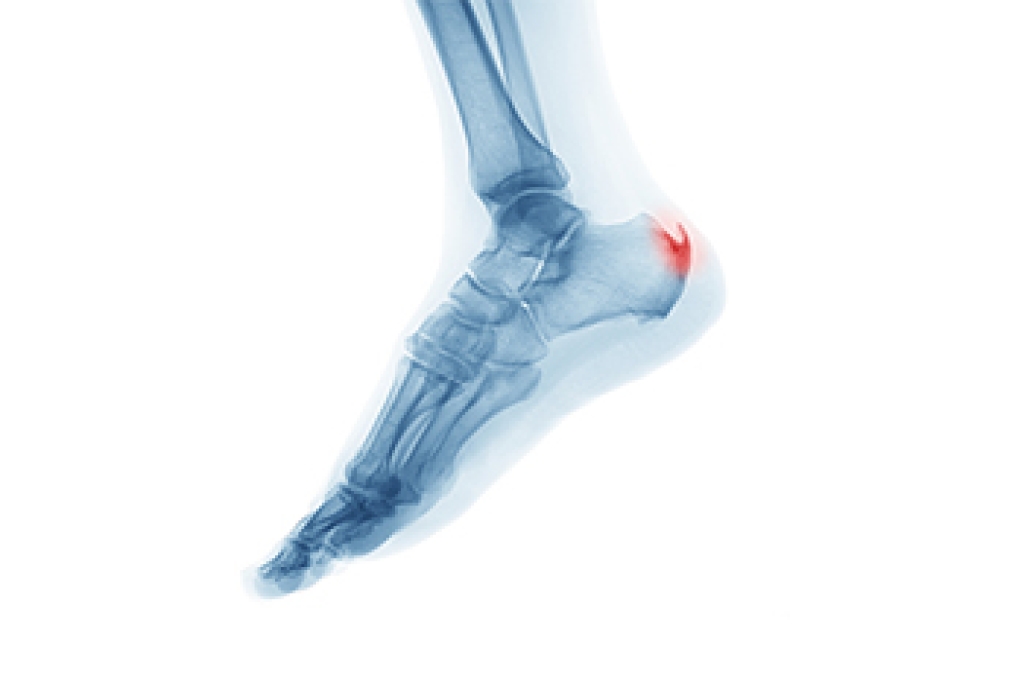
A heel spur is a bony growth that forms on the underside of the heel bone due to prolonged strain on foot muscles and ligaments. It often develops from repeated stress, inflammation, or tension on the plantar fascia. Although heel spurs are commonly associated with plantar fasciitis, they are not the same condition. Plantar fasciitis involves inflammation of soft tissue, while a heel spur is a calcium deposit on the bone. Some heel spurs cause no symptoms, but others can lead to sharp pain in the heel, especially when walking or standing. Discomfort may worsen after rest. A podiatrist can diagnose the condition and recommend appropriate treatment. If you have heel pain, it is suggested that you consult a podiatrist who can provide effective relief and treatment solutions.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact One of our podiatrists from Oexeman Foot and Ankle, PLLC. our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions, please feel free to contact our office located in Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.