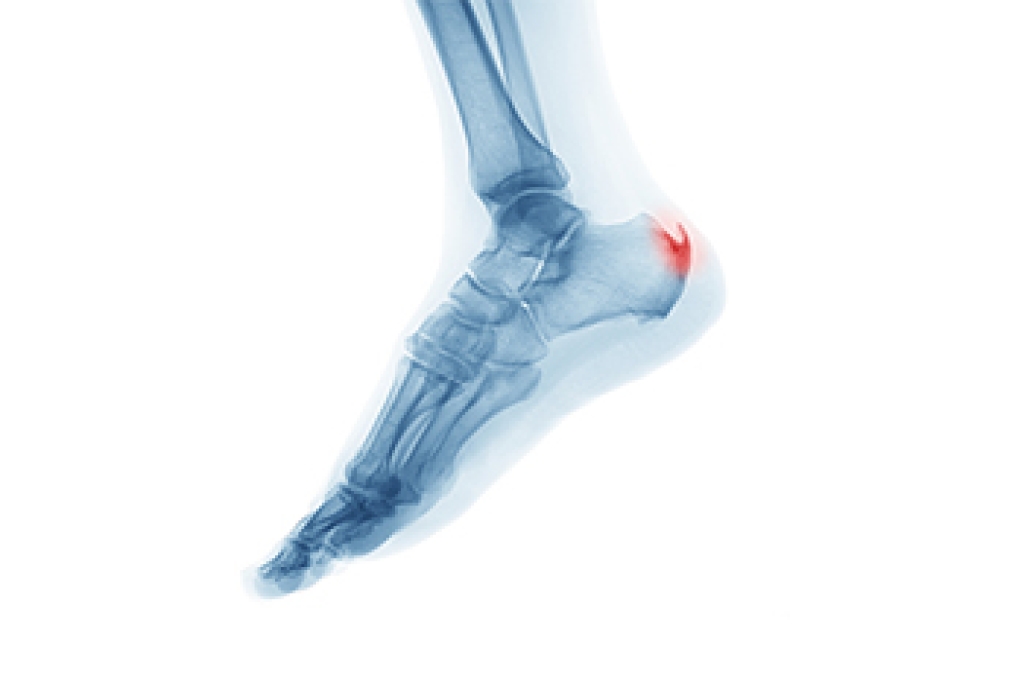
Gout is a form of inflammatory arthritis that often affects the joints of the feet and progresses through distinct stages. Asymptomatic hyperuricemia occurs when uric acid levels rise, but no pain or swelling is present. Acute gout is marked by sudden flare episodes with intense joint pain, redness, warmth, and swelling, commonly in the big toe. Intercritical or interval gout refers to the symptom-free periods between flares, even though uric acid crystals remain in the joint. Additionally, chronic tophaceous gout develops after years of repeated attacks and involves ongoing pain, joint stiffness, and firm crystal deposits that can damage bone and soft tissue. Early stages may seem manageable, but progression can lead to lasting joint problems. Identifying the stage helps guide appropriate care and long-term management. If foot joint pain or repeated flares occur, it is suggested that you see a podiatrist for appropriate care.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact One of our podiatrists from Oexeman Foot and Ankle, PLLC. our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions, please feel free to contact our office located in Chicago, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.